
‘If only doctors washed their hands!’
‘Cross-infection is spread by individuals, not be anonymous staff groups.’
‘Electronic hand hygiene monitoring systems…….. No, far too expensive for the NHS.’
Sound familiar?
The problem of maintaining high levels of staff HH performance are very well known by Infection Prevention and Control teams (IPCTs).
The issues are all too familiar
So is having the right AHHMS the answer?
Maybe, but the right system, which is fit for purpose for NHS staff, has proved elusive. Currently the uptake of AHHMS in hospitals is very low. Rightly so, as the cost of running a hospital-wide AHHMS has to be balanced by evidence of its cost-effectiveness in reducing preventable HCAIs.
Though there has been considerable commercial interest in AHHMS, there has been virtually no engagement with NHS staff as to what constitutes the right system and how AHHMS can be shown to pay for themselves. A light touch analysis of 12 current commercial systems against two essential criteria with a -4 to +4 rating scale is shown in the figure below.
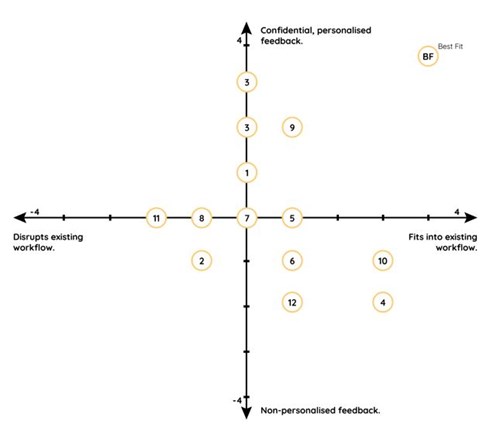
Figure: Analysis of commercial AHHMS by workflow and staff feedback
None of the existing systems were ideal when assessed in this way and the best fit solution remains elusive. Nevertheless, the fundamental objectives behind AHHMS remain attractive
So what is needed for an AHHMS to be useful for NHS staff?
Finally, the feedback has to be timely, non-judgemental and personalised with realistic individual improvement goals set for every member of staff. Everyone in the organisation should have feedback on their own HH performance.
Of course the monitoring system must also fit seamlessly into staff’s work pattern and must have no impact on staff workflow.
Such a system does not currently exist! However, there is no reason why such a system should not be developed.
Plugging the clinical research gap
In my work at Alder Hey’s Innovation Department, we are currently developing what we believe could be a “Best Fit” solution, as per the chart above. Still very much in development, we are actively looking for enthusiastic, like-minded Trusts to help us evaluate our innovative solution. This will involve a single Trust hospital-wide evaluation in partnership with University of Liverpool, to show the solution’s sustained impact on staff HH performance.
Published studies to date on AHHMS and HCAI reduction (which typically show 50% reductions in HCAI rates) fail to take account of other IPC initiatives which inevitably occur during any study period. Hence, in the long term, we are also planning a further evaluation with multiple hospitals to examine the solution’s true impact on HCAI reduction.
Call to action!
If you are interested or want further information, please contact me at richard.cooke@alderhey.nhs.uk
Richard Cooke
Consultant Medical Microbiologist/DIPC (retired) and Medical Founder at Alder Hey Children’s NHS Foundation Trust