
In May 2022, Dr Catherine Houlihan, a consultant in infection with UKHSA and consultant in clinical virology at University College London Hospitals NHS Foundation Trust, was awarded a HIS Small Research Grant. The project aimed to investigate the risk of Monkeypox virus transmission using cell culture as a proxy for infectiousness in clinical samples from patients diagnosed in the UK between 2018 and 2021. The project finished in July 2023. In this blog we spoke with Catherine to discuss her findings and her experience of being awarded a HIS Small Research Grant.
For this study, we originally planned to use left-over clinical samples from patients who had caught Monkeypox between 2018 and 2021. When the large global outbreak occurred, we added samples from patients infected in 2022. We investigated whether virus within these patient samples (urine, throat swabs, lesions, and blood) was still 'alive' and could infect people, by testing whether it was infectious to cells in the laboratory.

We found that infectious virus was present in some samples for up to 76 days after the patient first showed symptoms. The results show detection of 'replication competent' (i.e. potentially infectious) virus from nose and throat swabs, endotracheal swabs (the tube used to help someone breathe when they are unconscious) and urine. This has previously not been described. These are important findings which will inform isolation advice for patients, and infection control advice for hospitals.
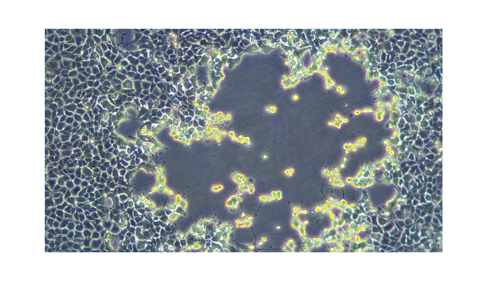
The study demonstrated that in two patients there was prolonged detection of potentially infectious Monkeypox virus in skin lesions up to day 25 and 76 days after symptom onset. This prolonged detection strengthens public health advice about reducing physical contact until lesions are fully healed.

The research resulted in a publication in March 2023 in the Journal of Hospital Infection entitled ‘Monkeypox virus isolation from longitudinal samples from four patients to infer risk of onwards transmission: an interim analysis’ (follow image link below to access the full paper). The updated results from 12 patients were also presented as a poster at the ECCMID 2023 conference in Copenhagen.
A further publication with full results from 12 patients (including the patient with prolonged detection) will follow.
Publications and invitations to discuss the work have assisted in improving and increasing my profile as an individual with expertise in high-consequence infectious disease infection control.
From being able to carry out this research, I have met and made connections with some excellent colleagues at UKHSA who share similar interests, and who carried out the laboratory testing in the Porton Down high containment facility. I was able to support a clinical fellow who led the project management and write up and, outside of UKHSA, I have expanded my network of colleagues and collaborators relevant to IPC and high-consequence infectious diseases, allowing further clinical and research opportunities.
The results speak for themselves: improved understanding of shedding and the infectiousness of this now common(!) virus.
Now that the network and collaborations are established, we will be able to repeat this work rapidly when a new pathogen outbreak occurs. We may require additional funding and HIS would be a group we would approach.
This was simple and rapid and the support from HIS was easily available. We made the initial application before the global Monkeypox outbreak but were able to speed things up when the public health importance rapidly became apparent given the evolving situation. I have learned a lot about the timings of funding release and the various signoffs required in my institution.
Go for it! This is a very approachable and pragmatic funding body who support timely and important work.